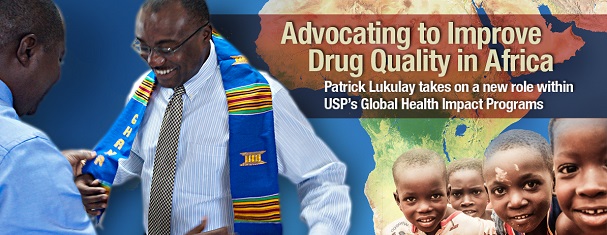
Not long after landing in Accra and assuming his new post at USP–Ghana, Patrick Lukulay, Ph.D., USP’s Vice President of Global Health Impact Programs–Africa, was at work, alongside his staff, partners, and allies doing what he’s most passionate about—breaking down barriers to the advancement of pharmaceutical quality in Africa.
These barriers have created an environment where poor quality medicines have flourished. But recently, Dr. Lukulay relocated to Ghana to be in a better position to change this. After spending over eight years at USP’s corporate headquarters in the United States, where he helped shape and nurture USP’s Global Health Impact Programs (GHIP) into what they’ve become today, he now plans to expand USP’s public health initiatives and enhance GHIP’s impact in Africa.
How will he accomplish this? Dr. Lukulay plans to engage and collaborate with stakeholders in Africa that are involved in aspects of quality assurance, quality control, and the regulation of medical products at local, national, regional, and global levels. Using advocacy to inspire change, influence policy and incite collective action, through his new role, he hopes to foster and expedite the removal of deep-seated challenges to sustainable progress in pharmaceutical quality in Africa.
So far, Dr. Lukulay and staff at CePAT have hosted an open house where they engaged and strengthened relationships with embassy representatives from various countries and the Ghana Ministry of Health. He was also the moderator of a summit in Mozambique at which regulatory agencies from Mozambique, Zambia, Nigeria, Ghana, Liberia, and Angola shared lessons learned and experiences combating counterfeit and substandard medicines and improving drug quality. Through these engagements, "we are breaking geographic boundaries, building capacity and forging partnerships across Africa."
Championing the Public Health Benefit of Quality-Assured Medical Products
To break down barriers to quality-assured medical products, Dr. Lukulay and his staff plan to embark on a new mission—one he calls "USP–AID in Africa.” It involves “Advocacy, Identifying areas of unmet need, and Designing programs to meet them."
Certain factors must exist to foster an environment that is conducive to change and primed for effective quality-assurance, quality control, and drug regulation—and can sustain them. As a champion for drug quality in Africa, Dr. Lukulay plans to help empower people and institutions with the awareness, knowledge, motivation, beliefs, skills, and resources that will enable them to develop strong drug quality systems that can carry out these functions and processes at local, national and regional levels throughout the continent.
Countering Fallacies that Deter Drug Quality
Part of Dr. Lukulay’s advocacy role involves debunking fallacies which have distorted the perception of drug quality in Africa, which include:
- Fallacy (1): Provision of any medicine is better than no medicine; Access is better than lack of access.
Dr. Lukulay: "Access to medicines does little to improve public health if the medicines we provide are not safe and quality-assured. The cost of poor quality medicines, which include wasted resources, failed treatments, lost lives, dismantled public health programs, and weakened health systems, are in fact, prohibitively very high and unacceptable."
- Fallacy (2): Quality is a luxury, not a necessity.
Dr. Lukulay: "In pharmaceutical and regulatory science, quality is not a luxury, but instead, it is a vital necessity. There is an undue focus on cost containment and less on quality improvement. Without quality-assured medical products, the inherent promise of medicines, that they will be safe and contain the ingredients intended for them to work, is lost. Hence, there is no guarantee that product will be safe, and therefore, trust, confidence, and reliance on medicines and the health programs and systems that provided them are lost."
- Fallacy (3): Meeting product specifications is a sufficient determinant of quality—the end justifies the means.
Dr. Lukulay: "This may be true in other fields, but in pharmaceutical manufacturing, the opposite is true—the means justify the end and guarantee the outcome. This is because, quality is not just controlled but it should be assured and built into the product. This is only done when process standards (Good Manufacturing Process (GMP)) are combined with product standards to assure products of consistent quality. Process standards are proxies for quality; they can help ensure that contamination is prevented in the manufacturing process (which is not controlled through quality control tests) and that quality products can be made consistently and reliably."
- Fallacy (4): GMP is not worth the expense to meet it.
Dr. Lukulay: "To state that GMP is not worth the expense to meet it is akin to saying that one should continue to ride a horse and not buy a car because it is expensive. In order to retain and expand their markets, manufacturers need to meet international standards of GMP. What’s good for the health of their people is also good for the health of their business."
What’s Next? Intensifying Efforts to Build a Stronger Regulatory Workforce in Africa
There is an acute shortage of trained regulatory personnel capable of conducting adequate regulation of medical products in Africa. USP–Ghana has a renewed interest in tackling this problem, and plans to intensify and expand its programs, as needed, to build a robust and viable regulatory workforce.
"There is urgent need for interventions that develop human capital for the effective regulation of medical products in Africa," says Dr. Lukulay. "Human resource development is a long-term process. High staff turnover due to unattractive remuneration, the highly dynamic field of regulation, and a lack of adequate training at the tertiary education level for regulatory workforce development are factors that complicate the workforce development process. They also make it difficult to sustain any gains in developing competent and capable personnel. It is now our vocation to help bridge the gap between the human resource needs and the availability of trained workforce that is capable of conducting key regulatory functions and helping to rid the market of falsified and substandard medical products."
"Being on the ground in Africa has taken me closer to the problem and has given me the opportunity to be in a better position to advocate, identify areas of unmet need and design more robust programs to meet the needs of ensuring drug quality in Africa."
Patrick Lukulay, Ph.D., is the Vice President for USP’s Global Health Impact Programs–Africa. He welcomes your comments below, or you can contact him by email at phl@usp.org. For more information on CePAT, its trainings, and plans for expansion and growth, email Dr. Lukulay or visit our website.


